Platelet Rich Plasma (PRP)
What is Platelet Rich Plasma (PRP)?
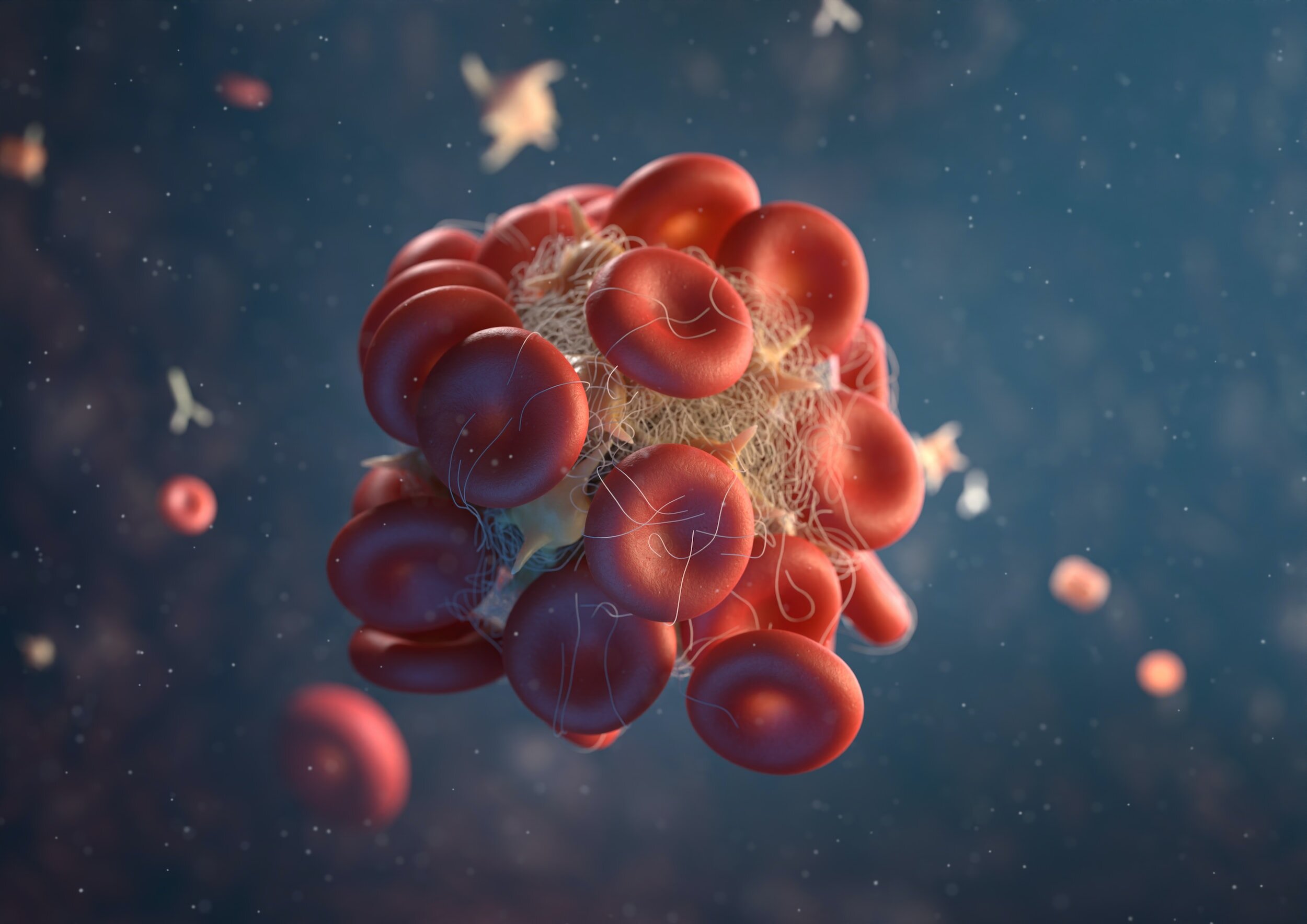
PRP is a concentrated solution derived from a patient's blood, specifically enriched with platelets, growth factors, and bioactive proteins that can enhance healing and reduce inflammation.
PRP may be injected directly into damaged tissue or joint during an outpatient procedure, or at the time of a surgical procedure following a repair.
The process involves isolating and concentrating these healing components from the patient's blood through centrifugation, creating a potent therapeutic solution.
What do Platelets do?
Platelets are one of the first biologic products to reach an injury. Their first function is to participate in sealing the injury with a clot. During the blood clot formation, they release over 1,500 biologically active proteins, including both growth factors and “signaling” factors (that recruit adult tissue-specific cells to aid in the repair process). These factors aid in initiating the healing response at a site of injury
PRP is thought to initiate or possibly accelerate the body's innate healing processes, promoting tissue regeneration, reducing inflammation, and fostering faster recovery from musculoskeletal injuries.
What is the science behind PRP?:
Osteoarthritis
Knee Osteoarthritis
Hip Osteoarthritis
Shoulder Osteoarthritis
Glenohumeral Osteoarthritis: The Role for Orthobiologic Therapies
Tendon Injuries
Gluteal Tendons (Trochanteric Bursitis)
Lateral Epicondylitis (Tennis Elbow)
Rotator Cuff Tendon (Tendinopathy and Partial Thickness Tears)
Distal Biceps Tendinitis
Common PRP Questions
-
Unfortunately, PRP injections are not currently covered by insurance. Most insurance programs, Medicare and Medicaid label PRP injections as “experimental or investigational” and do not pay for these treatments.
You will be required to pay for your PRP injection at the time of your treatment.
Consult with your Health Savings Account (HSA) adviser prior to your appointment, as prescribed medical treatments may be allowed for payments from your HSA account.
-
How your body responds to the PRP injection, unfortunately, is unpredictable. Following your PRP injection, most patients report improvement in two to six weeks. Some may have improvement within the first week while others may take up to six weeks to respond. If there is no response after six weeks, it’s likely the PRP injection was not effective.
-
The entire process for PRP will take about 30-45 minutes in total.
You will be required to stop taking aspirin and/or anti-inflammatory medications 1-2 weeks prior to the procedure as they have been shown to alter platelet function. It is recommended to avoid for 6 weeks after the injection as well.
Blood is drawn by a medical assistant.
Blood is placed into a centrifuge and the Platelet rich plasma layer is separated.
The physician will then cleanse the injection site and apply the local anesthetic to numb the skin around the injection site.
The injection is applied into joint/tendon, typically under ultrasound guidance.
-
Any time a needle is placed anywhere in the body, even getting blood drawn, there is a risk of infection, bleeding, and tendon and nerve damage. However, these are rare. Other complications, though rare, can occur depending on the area being treated and will be discussed by your physician before starting treatment.
-
After the initial treatment, a follow-up visit is scheduled 6 weeks later. Most patients respond well to just one treatment. However, additional treatments may be desired in some cases.
-
Because the injured area is first anesthetized with lidocaine, the actual injections can be slightly uncomfortable. The lidocaine wears off in a few hours, and there is usually mild to moderate pain for the next few days. Because the healing process is restarting and involves inflammation, some people may have increased pain for approximately a week after the injection. Then, over the next 5–6 weeks as the area goes through the healing process, symptoms improve.
-
Activity restrictions are typically reviewed with your physician on a case by case basis. In general you can resume normal activities immediately after the injection, but refrain from high intensity activities for a minimum of 2 weeks.
Additionally, for the first 6 weeks after the injection, it is recommended to avoid NSAIDs (ibuprofen, naproxen, celebrex, mobic, diclofenac, etc) as these can impact inflammation and healing after the injection. It is ok to utilize ice therapy and tylenol after the injection.
-
The overall success rate depends on the condition being treated along with the initial disease state. For example, patients with mild to moderate arthritis are more likely to receive benefit than those with advanced arthritis. Some patients can experience complete relief of their pain. No guarantees are made regarding treatment efficacy and literature studies are included above and you are encouraged to do your own research.
